Natural Solutions to Menopause
17th May 2019
There has been a lot in the news this week for ‘National Menopause Week’ but it predominately seems to surround the use of HRT. This may work well for some but what about for others who don’t want to use prescribed medication to help them through what is, after all, meant to be a natural progression in a woman’s life.
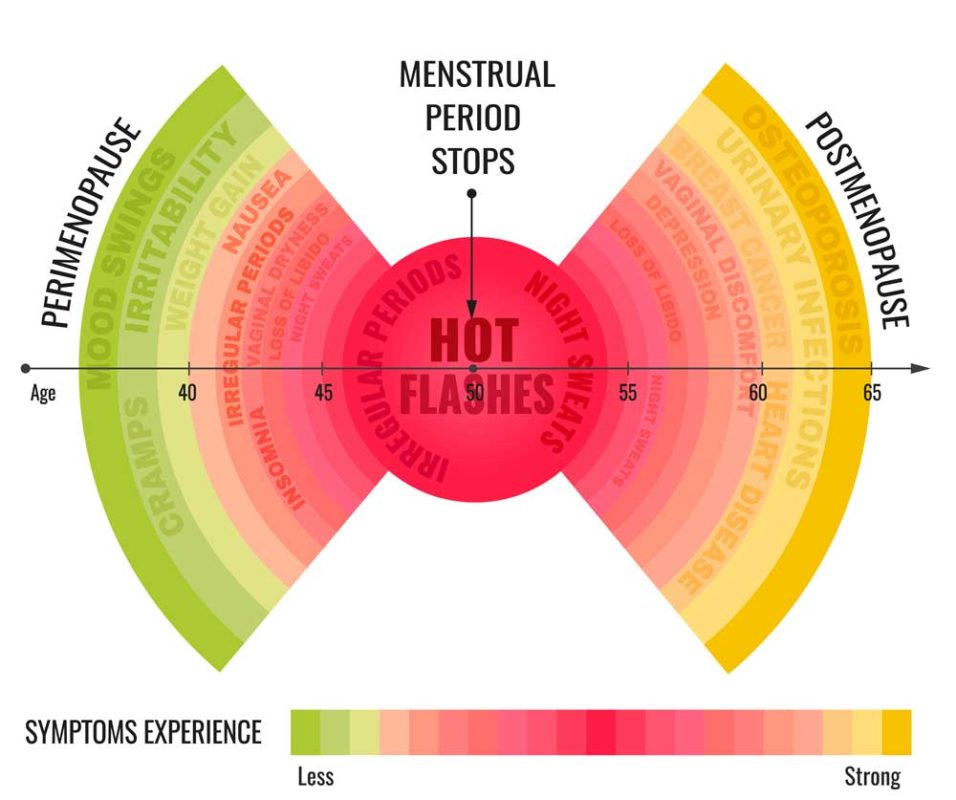
When a woman’s ovaries begin to wind down towards menopause, symptoms such as significant mood swings, hot flushes, night sweats, unusual weight gain and forgetfulness are commonly experienced which can be not only disconcerting but hard to manage. However, this, in theory, should be a stage one passes through and not, as we are now being led to believe, a serious medical condition. So, what is going on – why does one woman have severe symptoms and another none?
What I am going to do is explain a little bit from a functional perspective of why some woman experience more significant symptoms than others and what you can do about it if you are one of those women who is struggling. Or if you simply want to understand more in preparation for the years ahead.
As we age, the ovaries do not suddenly shut down production of oestrogen (or oestrodial to be more precise), it is a gradual decline during what is called the peri-menopause years when women typically experience irregularity in their cycles. In theory, the adrenal glands pick up some of the slack by aiding in oestrogen production via the production of oestrone (the predominant oestrogen in the body post menopause) and the body can convert some fat to oestrone.
Some Factors Influencing Menopausal Symptoms:
- Stress – via its impact on adrenal function. Stress comes in many guises and can typically be categorised as physical, physiological and psychological and stress affects adrenal function via what is commonly known as the ‘HPA’ axis. The HPA axis connects our hypothalamus (in our brain) to our pituitary glands, adrenal glands, ovaries and thyroid and they are all inter-connected by complex feedback loops. If these loops become dysregulated over a long period of time due to, say, chronically elevated cortisol, there are ramifications such as potential thyroid dysfunction and insulin resistance. Insulin resistance and menopause are closely associated as declining oestrogen can negatively impact cell insulin sensitivity resulting in a lack of metabolic flexibility. In addition, for the adrenal glands to pick up some of the slack and produce oestrone, they need to be able to produce adequate amounts of DHEA. This can be measured in a variety of ways and often found to be low in clients who are struggling with menopause symptoms. This can be due to a lack of raw materials (such as cholesterol) or the body’s HPA axis does not function properly from years of chronic ‘stress’.
- Cholesterol – many people, especially those around in the 1980’s who believed low fats diets were good and avoided all forms of cholesterol are now in their menopause years and still holding onto this long-held belief. Cholesterol is essential not only for healthy cell membrane function and thus communication between cells but it is the building block of both DHEA, cortisol and the androgenic sex hormones, such as all forms of oestrogen.
- FSH – or Follicle Stimulating Hormone. This is the hormone that stimulates oestrodial production in the ovaries and actually increases in the early years of the menopause. FSH has a dilating effect and its increase is thought to be one of the mechanisms behind hot flushes.
- Lack of Adequate Nutrients – all pathways require nutrients for raw materials and cofactors to work. Some of us need more than others due to genetic variations, different stressors we have in our lives and different environments. Ensuring your eat a diet that is right for you and supplement where necessary is important.
What can you do?
- Make some lifestyle adjustments – Learn to tap into your para-sympathetic system ie relax. This doesn’t mean you have to stop work or give up what you love doing but make sure you find time to wind down, start yoga, experiment with meditation or get a massage.
- Balance your blood sugar – imbalanced blood sugar can lead to elevated insulin and longer term insulin resistance which can exacerbate the potential lack of insulin sensitivity resulting from oestrogen decline. Improve your chances of avoiding a problem and abdominal weight gain by ensuring each meal is balanced with adequate amounts of protein, healthy fats and unprocessed carbohydrates (such as all forms of vegetables especially plenty of green leafy vegetables and other brightly coloured sources). Limit fruit to 1-2 pieces a day with a preference for berries due to their high antioxidant content and lower glycemic-load. Ensure other good sources of fibre in your diet and avoid processed foods where-ever possible.
- Fish oil – Fish oil (EPA, DHA, GLA) has been shown to be a useful supplement to help reduce hot flushes and something to consider especially if oily fish is low in your diet or you are vegan (vegan supplement sources are available).
- Vitamin C – is a necessary for optimal adrenal function and has also been shown to improve arterial function in post-menopausal women.
- Phyto-oestrogens – consider increasing your foods that contain phyto-oestrogens – such as non-GM fermented soy and flaxseed. Herbs such as sage, red clover, celery seed and alfalfa are also sources of phyto-oestrogens which have been shown to help reduce hot flushes and positively impact bone health (see health warning below).

- Vitamin E – has shown to be effective in reducing vaso-motor activity ie reducing the incidence of hot flushes. The best food sources of vitamin E are sunflower seeds, almonds, spinach, swiss chard and avocado.
- Exercise – in moderate forms (not necessarily Ironman or ultra-marathons) has been shown to have many beneficial effects on both peri and post-menopausal women such as reducing hot flushes, decreased bone loss, improved circulation, improved ability to deal with stress. Cardiovascular and strength based exercises are important as we age.
- Be Preventative – there is evidence that lower PMS symptoms in earlier years reduces the incidence of menopausal symptoms. Seek advice before the menopause hits to find out the root cause of your PMS.
I have not discussed here the potential risks and studies supporting, or otherwise, the links of HRT with increased risk of breast cancer as that is something I go through in detail with clients on a one-by-one basis to help put the risks versus benefits into context of their own unique situation.
Health Warning: Please also be aware that none of the above constitutes advise as every client must be assessed individually to find what is at the root of their symptoms and that if you are on medication, herbs can interact with these and advise from a suitably qualified healthcare practitioner should be sought.

–
This is a Guest Post by Katherine.
Katherine is a degree qualified Functional Nutritional Therapist in private practice at Brighter Spaces Islington. To see how a Functional Nutritional Therapist can help you, please visit www.kchnutrition.co.uk or contact Katherine directly at info@kchnutrition.co.uk.
